Recognising and Responding to Trauma: Recognise, Respond, Link

Model References
- *Hobfoll S. E, Watson P, Bell C. C, Bryant R. A, Brymer M. J, Friedman M. J, et al. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry. 2007;70:283–315.
- **Hughes, D.A. (2009) Attachment Focussed Parenting WW Norton: New York
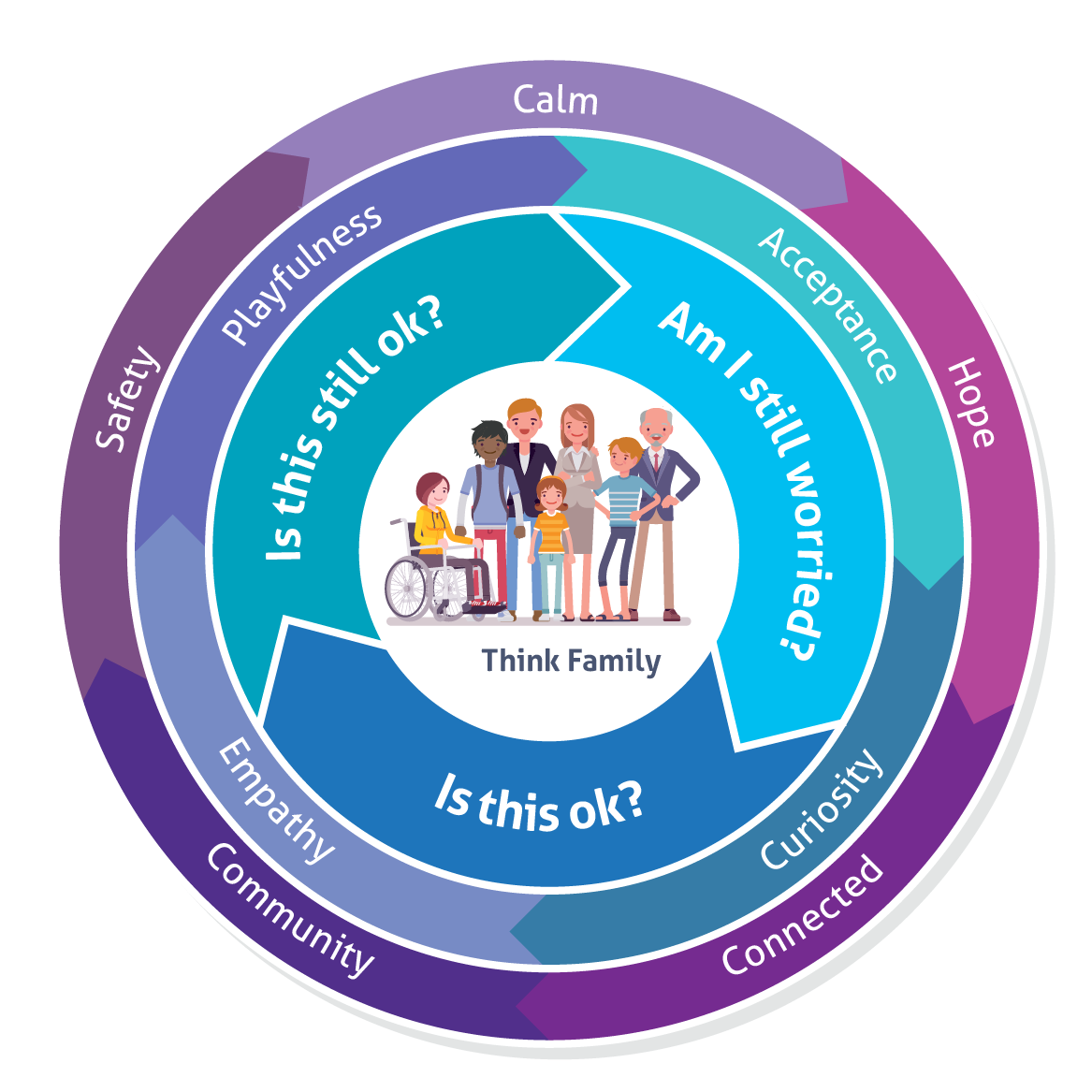
Over the past few years we have all experienced different emotions, changes to our routine, circumstances, family dynamics, changes in our schools or college, employment and income, some of us have experienced painful loss and grief and for some children and adults they have experienced war, terror and displacement. With all these changes we are experiencing most of the time, we may be able to manage with the right support around us, but we might sometimes wonder, along with everyone else, is this ok?
To help us recover from trauma experiences, a way of working has been developed to support children and adults which focuses on ensuring the right support at the right time and the prevention of need and risk. It is anchored in:
- The five essential principles of responding to trauma: calm, hope, community, connected, safety.
- PACE: playfulness, acceptance, curiosity, empathy (Dan Hughes **) This is a framework to help structure conversations.
- These build on our partnership way of working through trauma informed practice and motivational interviewing to build resilience, support recovery and celebrate success. It is a way of working which draws on person-centered practice to ensure that children and adults are truly listened to and are kept at the heart of all decision-making.
The partnership’s child protection and early help processes for referrals across the continuum of need for children and adult safeguarding have not changed. We have provided advice and guidance on accessing these services in the guide below.
• Continuum of need
• Children
• Adults
Changes in routines, stress and trauma can be seen through emotions, behaviours and physical health. Children and adults should receive the right support when they need it. The resource will help you as you may sometimes think …
There are three steps to using the guide:
Recognise, Respond, Link
Some of the main areas for you to recognise are detailed below, please click to expand.
For free briefings and training to support you visit training for you
-
Sleep
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Tiredness, exhaustion, changes to energy levels and poor concentration, irritation, mood swings, unmotivated, shows no interest. This can result from difficulty in getting to sleep and staying asleep.
Children- Self help: mymind
- Talk with the child/young person and/or their parent/carer to identify any sleep difficulties for them or wider family members.
- Has this been a previous concern? If so, how has this been addressed?
- A number of children with special educational needs (SEN) take medication to aid settling to sleep. Are they using it? Have they started using it? Is it still as effective?
- Maintaining a balanced sleep pattern will decrease your emotional vulnerability.
- Ask the young person to start by keeping a sleep diary. For a young child talk to their parent/carer about this.
- Have sleeping arrangements changed due to bedroom sharing? Are they sleeping in a bedroom, on a sofa, in their own home or with another relative or friend?
- Does the young person recognise their sleep routine as a problem? Are they awake at the same time as their peers? Is this the time that they can communicate online with their peers?
- For parents and carers The Sleep Charity
- Bedtime-Sleep
- Sleep – Regulation for bedtime
Adults
- Talk to them to identify any sleep difficulties.
- Keep regular sleep hours.
- Go to bed when you feel tired.
- Get up roughly at the same time each day.
- If lying awake do not force sleep, get up and do something relaxing and go to bed when sleepier.
- Self help:
- Live Well: Sleep
Children and Adults
- Suggest a balanced routine involving physical activity, rest and relaxation.
Is this ok?
Children
Adults
- Encourage trying different approaches to establish new sleep routine
- Every mind matters – Trouble sleeping?
- Sleep and tiredness
- Every Mind Matters
Is this still ok?
Children
- If the problem persists guided help and advice can be gained from the Starting Well Service
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate
Multi agency group supervision
Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If experiencing continued difficulties, consider:
One you
Kind to your mind - Persistent sleep difficulties contact GP practice.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Longer term sleep issues may indicate depression or anxiety contact Children and Young Peoples Community Mental Health Services (previously CAMHS) for advice and guidance
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Advise to speak to GP practice if prolonged difficulties and may indicate other mental health needs and or contact Cheshire and Merseyside Mental Help Crisis helpline on 0800 145 6485
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours: 01244 977 277)
-
Nightmares
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Nightmares
Nightmares are disturbing dreams associated with negative feelings, such as anxiety or fear that awakens you. Nightmares are common in children aged 3-6 years but can happen at any age. Upon waking up from a nightmare, it is normal to be acutely aware of what happened in the dream, and many people find themselves feeling upset or anxious. Physical symptoms like heart rate changes or sweating may be detected after waking up as well.
Night Terrors
Usually happen shortly after going to sleep, and last for several minutes. Night terrors are common in children aged between 3 and 8 years old, but can happen at any age. Night terrors do not involve a full awakening; instead, a person remains mostly asleep and difficult to awaken. If awakened, it is likely they will be disoriented. People who experience night terrors very rarely have any awareness of the episode.
Children- Self help: mymind
- Has this been a previous concern? If so how has this been addressed?
- These can all be okay and indicate normal brain processing -try and maintain a good sleep pattern (see section on sleep) and consider the stress management strategies and healthy emotional regulation.
- Provide reassurance and suggest noting changes over the coming weeks.
Adults
- For adults, nightmares are often linked, to stress, trauma or existing mental health needs.
Is this ok?
Children
Adults
- Encourage trying different approaches to establish new sleep routine
- Every mind matters
- Sleep and tiredness
Is this still ok?
Children
- If the problem persists guided help and advice can be gained from the Starting Well Service
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate
Multi agency group supervision
Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If experiencing continued difficulties, consider:
One you
Kind to your mind - Persistent sleep difficulties contact GP practice.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Can indicate previous trauma and be an indication of re-traumatisation talk to someone else who knows the child, contact Children and Young Peoples Community Mental Health Services (previously CAMHS)/GP for further advice and guidance.
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Speak to GP practice if prolonged difficulties and may indicate other mental health needs and or contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Appetite
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Changes in weight might be noted along with changes to energy levels and concentration.
Children- These can all be okay and indicate normal brain processing, provide reassurance and suggest noting changes over the coming weeks as well as:
- Talk to parent/carer and ascertain if there have been any changes to mealtimes, availability and quality of food.
- Has this been a previous concern?
- If so how has this been addressed?
- Has someone else been shopping/providing the food?
- Are they reliant upon food banks?
- Does the young person have any choice/control over the food that they are or are not consuming?
- Are mealtimes a difficult time in the family household?
- Is the young person eating alone or having to obtain their own food?
- Have the weight changes been discussed? Are they planned?
- Is the young person experiencing a sensory issue? (see below for further information).
- Explore body image and anorexic thinking using trauma sensitive language.
- Encourage healthy eating in school and at home.
- Consider access to breakfast club if available.
- Self help: healthy food swaps
Adults
- Promote healthy eating at home and work encourage to stay connected and talk to trusted person.
- Self-help: mental health awareness tips
Is this ok?Children
- Live Well
- Five ways to wellbeing
- For further information and advice contact the Starting Well Service
- Can talk to emotional literacy support assistant (ELSA) for advice or whole class topic on a healthy diet.
- Children and Young Peoples Community Mental Health Services (previously CAMHS) training videos for professionals
Adults
- This can be part of wider number of difficulties that can relate to emotional wellbeing and stress, signpost to:
– How to manage and reduce stress
– Live Well
– Five ways to wellbeing
Is this still ok?
Children
- Contact Starting Well for advice and guidance.
- For children with Autism Spectrum Disorder (ASD) and now weight loss consider early referral to Cheshire and Merseyside Adolescent Eating Disorder Service (CHEDS)
- Beat Eating Disorders
- Live Well
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning Conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If difficulties persist advise to contact GP practice.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider consultation or referral to Children and Young Peoples Community Mental Health Services (previously CAMHS) if linked to altered self-body image, low mood or anxiety or for increased concerns for appetite/weight loss contact Cheshire and Merseyside Adolescent Eating Disorder Service (CHEDS).
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- Partner contact: if you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and present acutely concerning emotional and mental health needs advice to contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Personal Hygiene
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Poor personal hygiene.
Not washing clothes.
Excessive/obsessive cleaning and checking.
Children- Consider using social stories to help start conversations to understand behaviour or personal hygiene, particularly for young children or a good resource for children with Autism Spectrum Disorder (ASD).
- Has this been a previous concern?
- If so how has this been addressed?
- Inform the young person about what you have noticed i.e. unpleasant odour, dirty clothes and ask if they have the ability/facilities to maintain their hygiene.
- Is their personal hygiene a priority to them? What is their home environment like?
- Is the young person or child experiencing a sensory issue or trauma response that is preventing them from being able to maintain their hygiene? Use trauma sensitive language to support this conversation. For a younger child talk to their parent/carer about this.
- Gently ask about routines and generally how they are.
- Remember motivational interviewing techniques or Next Step cards.
- Watchful wait.
Adults
- Self-help: as above encourage to stay connected
- Take notice: become aware of present, understand yourself, improve mental wellbeing.
Is this ok?Children
- Observe and monitor ensuring regular check ins.
- Can talk to school emotional literacy support assistant (ELSA) and use whole class teaching linked to increase in handwashing routines.
Adults
- Emotional health and wellbeing support:
Is this still ok?
Children
- Consider welfare for child and whole family.
- Check out the basics, do the family have clothes washing facilities, access to a shower/hot water?
- What has already been done to address this?
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
Multi agency group supervision
Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If concerns persist encourage to seek support from GP (Social Prescribing) practice.
- Consider if talking therapy could provide support.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- If poor hygiene is linked to low mood contact Children and Young Peoples Community Mental Health Services (previously CAMHS). If excessive cleaning/checking does not calm down in four to six weeks contact CAMHS.
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and present acutely concerning emotional and mental health needs contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Sensory seeking behaviours
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Biting, chewing, tapping, touching, anger/frustration, refusal.
Children- For those children who are non-verbal is this an expression of pain/anxiety? What are they trying to communicate?
- Ignore if possible or allow time in the day for a ‘sensory diet’.
- Enquire about the following:
– has this been a previous concern?
– if so how has this been addressed?
– if there are previous behaviours what does the child/young person find useful?
– what has been effective in the past? Talk to the child/young person/parent/carer if possible.
– if these are new behaviours do they occur at specific times of the day?
– are these behaviours distressing to the child/young person? Are they affecting other people? - Discuss with the child/young person/parent/carer any possible contributing factors, changes in structure/routine, care provider, current or history of trauma.
- Talk to the child/young person about adaptive behaviour techniques, engaging in purposeful activities, self-soothing, mindfulness, distraction.
- These short term solutions will not necessarily meet their core need but will help the child/young person to reduce and or prevent in using sensory seeking behaviours.
- Consider sensory checklist profiling and develop a shared plan to reduce/increase sensory stimulus.
Adults
- Can be a sign of stress or anxiety – encourage to support reducing these feelings:
Take notice become aware of the present, understand ourselves to support improving mental wellbeing.
Be active physical activity can improve mental health and support in managing stress and anxiety.
Stay connected encourage a sense of belonging and self-worth.
Is this ok?Children
- For children with Autism Spectrum Disorder (ASD) consider social stories at National Autistic Society
- Further advice as part of the multi agency map to support emotional health and wellbeing of children and young people (formally behaviour pathway).
- These behaviours may be due to a sensory deficit or trauma response.
Adults
- Support emotional health and wellbeing:
– Live Well
– Kind to your mind
– NHS top tips to improve your mental wellbeing
Is this still ok?
Children
- Consider if further support can be provided through initiating a multi agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If concerns persist encourage to seek support from GP (Social Prescribing) practice.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider consultation or referral to Children and Young Peoples Community Mental Health Services (previously CAMHS) if concerns persist
- If you have concerns contract Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and present acutely concerning emotional and mental health needs contact Cheshire and Merseyside Mental Help Crisis helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concern contact 0300 123 7034 (or out of hours 01244 977 277)
-
Physical presentations of stress
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Other than those mentioned above other physical signs might be noticed – headaches, stomach aches, needing the loo, increase in bowel movement, tight chest, spots, being pale, tics, etc.
Children- Ask about general wellbeing and consider physical illness, share information with parents/carer.
- Remember those children who are not verbal. How do they communicate they are uncomfortable? Ask those professionals who know the child well to support with this.
- Self help:
– five ways to wellbeing
– action for happiness - Has this been a previous concern, if so how has this been addressed?
- Talk to the child/young person about health promotion, diet, exercise, mood-altering drugs, relaxation and stress management, sleep, if concerns for a younger child talk to them and their parents/carers.
- Check out what the child or young person may be communicating to you.
- Have their circumstances at home changed?
- Are they living in a home environment which has recently changed/suffered loss or trauma or feels uncertain to them?
Adults
- Ask about how they are feeling use trauma informed language, acknowledge you can see they are not themselves.
- Encourage self-help:
– Take notice: become aware of the present, understand ourselves to support improving mental wellbeing.
– Be active: physical activity can improve mental health and support in managing stress and anxiety.
– Stay connected: encourage a sense of belonging and self-worth.
– Give: encourage to consider different ways to support mental wellbeing and manage stress.
Is this ok?Children
- Can discuss with school mental health first aider who can signpost if required.
- Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage to seek support:
– Live Well
– Kind to your mind
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- Contact Starting Well for advice and guidance or visit GP practice.
- Consider if further support can be provided through initiating a multi agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If concerns persist encourage to seek support from GP (Social Prescribing) practice.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Contact Children and Young Peoples Community Mental Health Services (previously CAMHS) if thought to be related to mental health concern
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and present acutely concerning emotional and mental health needs advise to contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Nervousness, worries, anxiety fear and phobia
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Nervousness, worries, anxiety fear and phobia.
Children- Self-help:
– Minded
– Anxiety Canada
– Mymind - Has this been a previous concern?
- If so how has this been addressed?
- Gently enquire about what specifically is worrying them. Reassure and provide common sense evidence to support the reassurance.
- Worries are likely to be about their safety or about others not near them – separation worry. Can they identify the ‘worry thought’?
- Do not excessively reassure. Distract and reflect back times when they are in a different or better mood.
- Consider using scaling tools to gauge how strong or weak the worry is e.g. Next Step cards
- Together plan response e.g. breathing, exit card, access to safe place.
- Plan and co-ordinate approach with family.
- Model that worries are ok and can be helpful and can be controlled by us.
- Focus on positive behaviours and engagement. Consider whole school approaches to emotional literacy and regulation e.g. worry box or mood checking boards.
Adults
- Encourage self-help: provide assurance. Most people feel worries, anxiety and fear in different periods of their lives it can impact on how you physical feel and mentally respond to situations around you.
– Take notice become aware of the present, understand ourselves to support improving mental wellbeing.
– Be active physical activity can improve mental health and support in managing stress and anxiety.
– Stay connected encourage a sense of belonging and self-worth.
Is this ok?Children
- Can discuss with school mental health first aider who can signpost if required.
- Resources available from:
– Cosmic Kids Yoga
– P.E. with Joe Wicks
– Super Movers - Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage to seek support:
– Live Well
– Kind to your mind
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- Consider consultation with your child and educational psychologist (CEP) or Children and Young Peoples Community Mental Health Services (previously CAMHS)
- Contact Starting Well
- Visit
– Brio Leisure - Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- Hearing voices or experiencing alterations in our sensory fields (Hallucinations) can be as a result of extreme stress and anxiety however it could also indicate the start of a serious mental illness and medical attention should be sought from the GP immediately. Advise can also be sought at any time from CWP’s Crisis Line 0800 145 6485.
Adults
- For further support visit:
– Kind to your mind
– Talking Therapies - Hearing voices or experiencing alterations in our sensory fields (Hallucinations) can be as a result of extreme stress and anxiety however it could also indicate the start of a serious mental illness and medical attention should be sought from the GP immediately. Advise can also be sought at any time from CWP’s Crisis Line 0800 145 6485.
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Schools: consider consultation with your child and educational psychologist (CEP).
- Contact Children and Young Peoples Community Mental Health Services (previously CAMHS) if thought to be related to mental health concern.
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and present acutely concerning emotional and mental health needs advise to contact: Cheshire and Merseyside Mental Help Crisis helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
- Self-help:
-
Poor concentration
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Poor concentration, shows little interest, disengages and distracted easily
This might be linked to several of the above issues: worries, anxiety, fear, sensory changes, sleep for example.
Children- Has this been a previous concern? If so how has this been addressed?
- Explore reasons underpinning concentration issues.
- Routines and regular predictable breaks and changes in activity.
- Does the child or young person have a history of trauma?
- Are they living in a home environment which has recently changed/suffered loss or trauma or feels uncertain to them?
Adults
- Encourage and support mental wellbeing exploring a number of different approaches:
– Take notice become aware of the present, understand ourselves to support improving mental wellbeing.
– Be active physical activity can improve mental health and support in managing stress and anxiety.
– Kindness strengthens relationships, develops community and deepens solidity.
Is this ok?Children
- Can discuss with school mental health first aider who can signpost if required.
- Can talk to school emotional literacy support assistant (ELSA) who can signpost/advise as required.
Adults
- Encourage self-help:
– Live Well
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- Further advice as part of the multi agency map to support emotional health and wellbeing of children and young people (formerly behaviour pathway).
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If further support is needed:
– Kind to your mind
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider consultation with your child and educational psychologist (CEP).
- Consider Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation.
- If you have concerns contact Cheshire and Merseyside Mental Help Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Adult safeguarding concerns contact on 0300 123 7034 (or out of hours 01244 977 277)
- Contact GP practice
-
Changes in emotion
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Presentation and regulation vary from person to person and over time, often this is most visible through our behaviours for example from excitement (especially for young children) to sadness, feeling low and a sense of loss.
Children- With all behaviours it is important to try and find the meaning – what message/messages are being conveyed?
- Remember to try different ways depending on the normal way a child communicates. Is this by visuals, signing or by showing crying/laughing? Use the member of staff they communicate with best or the one who understands them most.
- Ask if this has been a previous concern? If so how has this been addressed?
- For schools supporting children and young people into new routine and new school environment may show different behaviours and emotions that may not be ‘compliant or containable’ but reflect how they are processing the changes around them.
- Consider PACE and how this could support your conversations and work with them.
- Consider motivational interviewing or Next Step Cards to explore change.
- Thoughtful observation, can you see any patterns or triggers, consider the impact of trauma and take a trauma informed approach
- What makes it better or worse?
Adults
- You may notice different emotions at different times and not a consistent regulated response, these can range from for example, increased alertness, denial, panic, avoidance, difficulties in managing change.
- Apply thoughtful observation, can you see any patterns or triggers, consider the impact of trauma and take a trauma informed approach
- Support the person to:
– Stay connected encourage a sense of belonging and self-worth.
– Take notice become aware of the present, understand ourselves to support improving mental wellbeing.
If you have explored different approaches for a family and things continue to remain the same for them – move to another section of the guide or advise them to speak to their GP.
Is this ok?
Children
- Can discuss with school mental health first aider who can signpost if required
- Can talk to school emotional literacy support assistant (ELSA) who can signpost/advise, as required for calming relaxation techniques
- Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage self-help:
– Live Well
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- Consider consultation with your child and educational psychologist (CEP)
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- For further support:
– Kind to your mind
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Contact Children and Young Peoples Community Mental Health Services (previously CAMHS) if thought to be related to mental health or contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i- ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and increase concerning emotional and mental wellbeing contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Withdrawn behaviours
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Withdrawn behaviours, for example do not talk like they used to and prefer their own company, reluctant to leave their room or home, socially withdrawn, increasingly more isolated from day to day activities.
Children- Has this been a previous concern?
- If so how has this been addressed?
- Were they reluctant to go to school and now this is much worse?
- Consider attachment difficulties if a parent has been unwell.
- How long has the child been withdrawn?
- Have other members of the family/ school noticed?
Adults
- Have other members of family, friends or work colleagues noticed?
- Support the person to:
– Take notice become aware of the present, understand ourselves to support improving mental wellbeing.
Children and adults
- Can you link the start of this withdrawn behaviour to a specific event?
- Are there any patterns or triggers to the behaviour?
- Can you ask them how they feel?
- Can they tell you how they feel?
- Draw on trauma informed language, consider using motivational interviewing
If you have explored different approaches for a family and things continue to remain the same for them – move to another section of the guide or advise them to speak to their GP.
Is this ok?
Children
- Consider how you can help them come to terms with the event. What seems to help? When is the child not or less withdrawn?
- Can discuss with school mental health first aider who can signpost if required.
- Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage self-help:
– Live Well
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- If there are continued concerns talk to school staff who may discuss possibility of intervention with school emotional literacy support assistant (ELSA) or a consultation with their child and educational psychologist (CEP).
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- For further support visit:
– Kind to your mind
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider consultation with Children and Young Peoples Community Mental Health Services (previously CAMHS) or Starting Well
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- If concerns persist and increase concerning emotional and mental wellbeing advice contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Sad and low in mood
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Sad and low in mood people may find their minds are preoccupied with negative memories, a bleak view of the future or negative thoughts about themselves or their current situation. They might withdraw from others, lack motivation or energy and feel like nothing is enjoyable. They might be tearful and experience thoughts of hurting themselves but equally the sadness might present as irritability or detachment or putting on an act that it’s all OK.
Children and Adults- Has this been a previous concern?
- If so how has this been addressed?
- Explore with the person what might be leading them to feel low. If they can identify reasons those reasons may indicate a problem that can be solved/ something they can change or something they need help to cope with.
- Self help:
Children – Mymind
Adults – Wellbeing, Self Help and Apps - Children – Have regular check ins with consistent staff members.
- Adults – Do they have a supportive friend, family member or support person they can talk to?
- Do not overly use rating tools.
- Encourage development of a self-help plan – exercise, mindfulness, journaling.
- Ask if they are having active thoughts about suicide and consider safeguarding, talk to your designated safeguarding lead in your organisation.
- Reflect and note times when mood lifts – do more of what works.
If you have explored different approaches for a family and things continue to remain the same for them – move to another section of the guide or advise them to speak to their GP
Is this ok?
Children
- Can discuss with school’s mental health first aider who can signpost if required.
- Can talk to school emotional literacy support assistant (ELSA) who can signpost/advise, as required.
- Resources available from:
– Starting Well
– Kooth
– Children and Young Peoples Community Mental Health Services (previously CAMHS)
– Brio Leisure
– NHS OneYou
– Cosmic Kids Yoga
– P.E. with Joe Wicks
– Super Movers - Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage self-help:
– Live Well
– Mind: wellbeing - Every Mind Matters
Is this still ok?
Children
- Consider consultation with child and educational psychologist (CEP).
- Contact Papyrus for help and advice for professionals, anyone who is worried about someone.
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047.
Adults
- For further support:
– Kind to your mind
– Sane - Speak to your GP Practice
- Western Cheshire IAPT: Further information and support
- Western Cheshire IAPT: Self-Referral and How to get help
- Cafe 71: A safe space for people struggling with emotional and psychological distress
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Children and Young Peoples Community Mental Health Services (previously CAMHS) referral if issues endure or have significant impact on engagement in school.
- Consider a multi-agency admission prevention meeting. If they have a diagnosis of Autism Spectrum Disorder (ASD) and/or learning disabilities and still at risk after this consider a Care, Education and Treatment Review (CETR)
- Children and Young Peoples Community Mental Health Services (previously CAMHS) training videos for professionals
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977277)
Adults
- If concerns persist and increase concerning emotional and mental wellbeing contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Speak to your GP Practice
- Western Cheshire IAPT: Further information and support
- Western Cheshire IAPT: Self-Referral and How to get help
- Cafe 71: A safe space for people struggling with emotional and psychological distress.
- If the person you are concerned about (or someone they care for) has additional needs or vulnerabilities, e.g. maintaining continence; staying safe or preparing food, they may benefit from an assessment under the Care Act and should contact Cheshire West and Chester, Adult Social Care, Community Access Team: Community Access Team
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Loss and grief
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Feelings of loss, grief, isolation and sadness.
The magnitude of loss is broad and deep from loss of a loved one, school routine and structure, unexpected endings, not taking exams, a job, not able to be with family and friends.
Many behaviours and experiences can be associated with loss and grief. It changes mood, presentation and behaviour (age related):
- Struggles eating and sleeping or comfort eating and sleeping a lot.
- Presentation of separation anxiety.
- Presentation of social anxiety – worried about going out and meeting others.
- Jumping in and out of feelings of loss, sadness and grief.
- Worried about illness and death.
- Some regressive behaviours.
- Presenting angry, aggressive and controlling (presenting subdued and disconnected).
- Reluctant to talk about feelings.
- Engaging in risky behaviours.
ChildrenTalking to children about the impact of loss:
- Lots of national and local support
- Have the child/young person and their family experienced loss and grief previously? Consider how this could be impacting further on them now.
- Prepare children before they return to school by using social stories.
– mainstream classroom
– comic strips - Children’s understanding of death at different ages
- Consider what supported them previously and if this would be appropriate to draw on again?
- Provide:
– re-assurance
– routine, structure and boundaries in place (knowing what to expect)
– warmth, comfort - “Normalising” feelings of loss and grief.
- Engaging children and young people in activities or with key people.
- Talking openly, naming the feelings and connections.
- Offering safe spaces to share, express, talk about feelings – personalise to child/young person’s needs (be creative: play, art, drama, dance, music, journaling, physical release, exercise, mindfulness, grounding).
- Talking factually about what’s occurred and impact (age appropriate).
- Allow short term dependence, regression.
- Encourage time with friends.
Adults
- Positive role-modelling.
- Engage in activities mentioned above.
- As and when helpful or needed support the adult in the above.
Is this ok?Children
- Can talk to school emotional literacy support assistant (ELSA) who can signpost/advise as required. It might be for six months to a year that children experience these emotions and behaviours.
- Mental health resource pack for schools.
- Managing unexpected endings and transitions
- Child Bereavement UK: supporting pupils
- Bereavement related links and resources:
– Hospice of the Good Shepherd - The Hospice of The Good Shepherd, the Hospice is offering Story Time sessions for under 8s (online). For more information, please contact Reflect@hospicegs.com– Reflect Children’s Bereavement Service
– Facebook
– Rip Rap (support for young people with parents diagnosed with cancer)
– Childhood Bereavement Network
– Grief Encounter
– Sesame Street – when families grieve
– Cruse Bereavement Care
– St Luke’s Children Bereavement Service
– Winston’s Wish UK
– Young Minds
– Child Bereavement UK
– Elsie Ever After
– Grief Encounter for bereavement support
– Hope Again - UK Trauma Council – Traumatic Bereavement Resources
Adults
- Mind
- NHS Grief after bereavement or loss
- Online Bereavement Help Point on zoom on the 1st & 3rd Monday of each month at 6:00pm and 2nd & 4th Wednesday of the month at 11:00, all welcome, email bereavement@hospicegs.com to register for a session
- The Hospice of The Good Shepherd Help Points offer, a Journal Group is running from January 2021, twice a month. Please, contact bereavement@hospicegs.com for more information and to book a place.
- Adult Bereavement Service
- St Luke’s Hospice Bereavement Service
– referral
– facebook - Survivors of Bereavement by Suicide
- SANDS: Stillbirth and neonatal death charity
Is this still ok?
Children
- GP practice, public health nurse for advice and guidance.
- Reflect Children’s Bereavement Service
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversations - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- Advise to contact GP practice.
- Adult Bereavement Service
- St Luke’s Hospice Bereavement Service
– referral
– facebook
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider Children and Young Peoples Community Mental Health Services (previously CAMHS) referral/consultation
- Counselling for emotional support
- Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Reflect Children’s Bereavement Service
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- St Luke’s Hospice Bereavement Service
- Family Support at Hospice of The Good Shepherd
- Cruse Bereavement Care
- If concerns persist and/or increase contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Angry, frightening behaviours
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Angry behaviours including shouting, hitting out, kicking.
Frightening Behaviour
- Raised, scary tone of voice
- Use of emotionally hurtful language
- Tense body language, facial expression and clenched fist(s)
- Physical harm – hitting
Children- Has this been a previous concern for the child or young person?
- If so, how has this been addressed?
- How long has the child or young person been presenting with frightening behaviour?
- Have other members of the family/ school noticed?
- Can you link the start of this frightening behaviour angry to a specific event? What are the triggers?
- Can you ask them how they feel?
- Can they tell you how they feel?
Adults
- Have other family members, friends, work colleagues noticed anything?
- Take notice: become aware of the present, understand ourselves to support improving mental wellbeing.
- Draw on trauma informed practice and consider root causes to anger considering childhood experiences, what is happening a person’s life in the present and what has happening in the past.
- Consider what has triggered the anger, encourage to discuss with someone they feel safe with.
- Is anger directed towards others or self?
- Does this place others or themselves at harm?
- Ensure that the person and those around them remain safe.
- If you have concerns talk to your safeguarding lead and follow safeguarding policies and procedures for children and adults.
Is this ok?Children
- Consider how you can help them come to terms with the event that happened before the anger started. What seems to help, when are they less or not angry?
- Can discuss with school mental health first aider who can signpost if required.
- Young minds – parents guide to support anger
- Person-centered practices are used with people to make sure that they are truly listened to.
– Person-centered thinking tools
Adults
- Encourage self help:
– Mind: causes of anger
– NHS: controlling anger
– Mood Juice: anger - Every Mind Matters
Is this still ok?
Children
- If there are continued concerns, talk to school staff who may discuss possibility of intervention with school emotional literacy support assistant (ELSA) or a consultation with their child and educational psychologist (CEP).
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– multi agency group supervision
– learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- Consider seeking further support and counselling.
- Anger associated with grief and loss consider:
– Cruse Bereavement Care
– St Luke’s Hospice Bereavement Service
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Anger may indicate issues with emotional regulation and mental health, consider consultation with Children and Young Peoples Community Mental Health Services (previously CAMHS).
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Contact GP practice as this may indicate concerns for mental health and emotional wellbeing.
- If concerns persist and increase concerning emotional and mental wellbeing advice contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Self injury and harmful behaviours
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Harmful behaviours might include cutting, burning or overdosing and may actively be behaviour which is helping the person manage difficult emotions and stressors. They may not be willing or able to stop. It may also include risk taking activity such as using alcohol or illicit substances (see below).
It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
Children and Adults- Consider safeguarding policy as a priority and talk to the designated safeguarding lead in your organisation.
- Do they require urgent specialist support to address suicidal thoughts and or their immediate physical wellbeing need attending to? (see Link column – Am I still worried?)
- Do they require intervention to clean the self-harm wounds?
- If they are willing to talk, gently engage using motivational interviewing approaches in your conversation, talk to them about how they are coping, explore the thoughts behind the behaviour including suicidal thoughts.
- Try not to make assumptions about the behaviour but be alongside to support if change is being considered.
- Suicidal thoughts need referral to partners in health (see advice in Link column).
- Has this been a previous concern?
- If so, how has this been addressed?
- If they are previous behaviours what did they find useful? What has been effective in the past?
- Are these new behaviours?
- Do they occur at specific times of the day?
- Consider family and friend support.
- Are these behaviours distressing for them?
- Are they affecting other people?
- Discuss with them and those that support/provide care for them any possible contributing factors, changes in structure/routine, care provider?
- Have they experienced trauma in the past or currently experiencing trauma, stress, changes, pain and or loss?
- Consider if they have a sensory need that is not being met?
- Talk to them about how they could start to change some of their ways of managing their pain and emotions through adaptive behaviour techniques, engaging in purposeful activities, self-soothing, mindfulness, distraction.
- These short term solutions will not necessarily solve the deep root of their pain and meet their core need but will help them to reduce/prevent harmful behaviours.
- Try and develop a shared safety plan with them.
- See each episode as new and re-assess for risk, try not to make assumptions from previous experiences, modify and update the risk plan and be mindful of confidentiality and preserving dignity.
- Children: Monitor and check in regularly and access supervision and consultation with CAMHS/safeguarding.
- Adults: Do they have a supportive friend, family member or support person they can talk to?
Self help:
Is this ok?Children
- Can discuss with school mental health first aider who can signpost if required.
- Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation and possible referral.
- Starting Well Service
- Mind Ed
Adults
- Self help tools and resources
- Cafe 71: A safe space for people struggling with emotional and psychological distress.
Is this still ok?
Children
- If concerns persist and increase contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation and referral when associated with changes in the behaviour e.g. becoming more frequent or when accompanied with suicidal thoughts.
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If concerns persist and increase contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- Self help tools and resources
- Cafe 71: A safe space for people struggling with emotional and psychological distress
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Does the child/young person require urgent specialist support to address suicidal thoughts and behaviours?
- Cheshire and Merseyside Mental Health Crisis Helpline 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation and referral when associated with changes in the behaviour e.g becoming more frequent or when accompanied with suicidal thoughts.
Safeguarding Concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01277 977 277)
Adults
- If concerns persist and increase contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- If the person you are concerned about (or someone they care for) has additional needs or vulnerabilities, e.g. maintaining continence; staying safe or preparing food, they may benefit from an assessment under the Care Act and should contact Cheshire West and Chester, Adult Social Care, Community Access Team: Community Access Team
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Thoughts of suicide
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Suicide means to end your life intentionally. Experiencing thoughts of suicide can be frightening. Thoughts of suicide can seemingly come from nowhere or begin as fleeting thoughts of wanting to disappear or escape. They may progress into feelings of hopelessness and worthlessness and planning or taking steps to end your life.
If someone is experiencing thoughts of suicide, it’s important they know that there is help available. Take some time with them to think about who they may want to talk to; maybe someone they trust or feel would understand them. It is important that they don’t have to carry these feelings on their own.
They will need emergency help if they have already taken steps to end their life or if they have thoughts of suicide which are particularly intense right now and they feel unable to stay safe from suicide.
To get emergency help, they can visit their local A&E department or call NHS 111 (England, Scotland, N. Ireland), NHS Direct (Wales)* or 999 and ask for some support.
NHS 111/ Direct can advise about where to get help such as a walk-in centre or an out of hours doctor. They may also have information about ‘safe spaces’ to access in their local area for when they are struggling to stay safe from suicide.
999 can support in an emergency too, the operator can advise about different types of immediate support the emergency services can offer.
Children
- Monitor and check in regularly and access supervision and consultation with Children and Young Peoples Community Mental Health Services (previously CAMHS)/safeguarding.
Adults
- Do they have a supportive friend, family member or support person they can talk to?
Children and Adults
- Do they require urgent specialist support to address suicidal thoughts and or their immediate physical wellbeing need attending to? (see Link column – Am I still worried?)
- Do they require intervention to tend to any self-harm wounds?
- Consider safeguarding policy as a priority and talk to the designated safeguarding lead in your organisation.
- If they are willing to talk, gently engage using motivational interviewing approaches in your conversation, talk to them about how they are coping, explore feelings behind the suicidal thoughts.
- Has this been a previous concern?
- If so, how has this been addressed?
- Consider family and friend support.
- Discuss with them and those that support/provide care for them any possible contributing factors, changes in structure/routine, care provider?
- Have they experienced trauma in the past or currently experiencing trauma, stress, changes, pain and or loss?
- Consider if they have a sensory need that is not being met?
Talk to them about how they could start to change some of their ways of managing their pain and emotions through adaptive behaviour techniques, engaging in purposeful activities, self-soothing, mindfulness, distraction.
- These short-term solutions will not necessarily solve the deep root of their pain and meet their core need but will help them to reduce/prevent harmful behaviours.
- Try and develop a shared safety plan with them.
See each episode as new and re-assess for risk, try not to make assumptions from previous experiences, modify and update the risk plan and be mindful of confidentiality and preserving dignity.
Is this ok?
Children
- You can discuss with school mental health first aider and/or Mental Health in School Team (MHST) key worker who can advise and signpost if required.
- – Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation and possible referral
- – Papyrus
- – YoungMinds
- – The Mix
- Useful Resources – No More Suicides (no-more.co.uk)
Adults
- – Self-help tools and resources
- – Calm
- – Samaritans
- – Cafe 71: A safe space for people struggling with emotional and psychological distress.
- Useful Resources – No More Suicides (no-more.co.uk)
Is this still ok?
Children
- If concerns persist and increase contact Cheshire and Wirral Mental Health Crisis Helpline on 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- Children and Young Peoples Community Mental Health Services (previously CAMHS)consultation and referral when associated with changes in the behaviour e.g. becoming more frequent or when accompanied with suicidal thoughts.
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- If concerns persist and increase contact Cheshire and Wirral Mental Health Crisis Helpline on 0800 145 6485.
- It’s important for anyone who self-harms to see their GP. They can treat any physical injury and recommend further assessment, if necessary.
- Self-help tools and resources
- Cafe 71: A safe space for people struggling with emotional and psychological distress
Am I still worried?
Children
- Does the child/young person require urgent specialist support to address suicidal thoughts and behaviours?
- Cheshire and Wirral Mental Health Crisis Helpline 0800 145 6485
- Visit your local A&E department or call NHS 111 (England, Scotland, N. Ireland), NHS Direct (Wales)* or 999 and ask for some support
NHS 111/ Direct can advise you about where to get help such as a walk-in centre or an out of hours doctor. They may also have information about ‘safe spaces’ you can access in your local area when you are struggling to stay safe from suicide.
999 can support you in an emergency too, the operator can talk to you about different types of immediate support the emergency services can offer
Safeguarding Concerns:
Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
Does the adult require urgent specialist support to address suicidal thoughts and behaviours?
Cheshire and Wirral Mental Health Crisis Helpline on 0800 145 6485.
Visit your local A&E department or call NHS 111 (England, Scotland, N. Ireland), NHS Direct (Wales)* or 999 and ask for some support
NHS 111/NHS Direct can advise you about where to get help such as a walk-in centre or an out of hours doctor. They may also have information about ‘safe spaces’ you can access in your local area when you are struggling to stay safe from suicide.
Safeguarding concerns:
If the person you are concerned about (or someone they care for) has additional needs or vulnerabilities, e.g. maintaining continence; staying safe or preparing food, they may benefit from an assessment under the Care Act and should contact Cheshire West and Chester, Adult Social Care, Community Access Team: Community Access Team
999 can support you in an emergency too, the operator can talk to you about different types of immediate support the emergency services can offer
Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Caring for someone close to you
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …This could be young carers caring for a parent, sibling, family member, or an adult caring for a partner, their child, sibling, parent or older adult.
Many people who are caring for someone wouldn’t describe themselves as carers but as a wife, husband, mother, father, son, daughter, close relative, good neighbour or friend. Looking after each other is something they do.
Caring can be very rewarding, but can also be challenging, especially at the moment during the Covid-19 outbreak when many people are spending more time caring than usual. Many carers are feeling overwhelmed by the current situation. Without the right support caring can be tough and can have a negative impact on physical and mental health, work, finances and relationships.
Children- Take a ‘Think Family’ approach:
– Talk to the child/young person.
– Talk to wider family members. - Understand the whole family situation:
– Consider who else is in the family home?
– How is the child/young person managing in their caring role?
– Do they need any additional support?
– Consider if local services could offer support.
Adults
- A carer’s assessment can enable carers to connect to a range of local help, support and advice. It can also help practically with equipment, support for their own wellbeing and can also arrange a break from caring.
- Top tips for carers:
- Tell your manager you are a carer and read the employer guidance on supporting you with your caring responsibilities
- Call the carer helpline for help and support – 0300 102 0008
- Make sure you’re accessing all the benefits/grants that you are entitled to
- Connect with your community
- Ask your local authority about a Carers’ assessment
- Look after yourself – your physical mental health and wellbeing are important
- Know your rights as a carer
- Tell your GP you’re a carer
- Remember, if you juggle work with looking after someone at home, you are still a carer!
Is this ok?Children
Adults
Is this still ok?
Children
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- Contact the dedicated helpline to provide advice and support, and where necessary make arrangements for food, medicines and social contact. Call 0300 123 7031 or email enquiries@cheshirewestandchester.gov.uk
- Cheshire and Warrington Carers Trust can help with practical support about where to find information, how to get a carers’ assessment and advice about finances and benefits. They can also provide a listening ear if you are finding things tough and just need to talk to someone. Call 0300 102 0008 or email advice@cheshireandwarringtoncarers.org
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Mymind: crisis
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- If the person you are concerned about (or someone they care for) has additional needs or vulnerabilities, e.g. maintaining continence; staying safe or preparing food, they may benefit from an assessment under the Care Act and should contact Cheshire West and Chester, Adult Social Care, Community Access Team: Community Access Team
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
- Take a ‘Think Family’ approach:
-
Domestic abuse
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Children
Children and young people may show us how they are feeling in different ways through their behaviour for example:
- May have nightmares, bed wetting, complain of physical symptoms such as tummy aches.
- Feeling confused, withdrawn, low mood, anxious, angry, afraid, isolated, ashamed, guilty, low self esteem.
- Be unable to concentrate and struggle in achieving in school.
- Be used to threaten the adult victim (threats to harm children or have them taken into care).
- Protective of family members.
- Risk getting hurt by being caught in between parents.
- Not have their own needs fully met by a parent who is struggling to cope with being abused.
- Be directly abused by the person who is harming the adult.
- Showing signs of trauma being in fight or flight.
- Develop ways of coping that could hurt them and show their distress e.g. running away or using substances.
Contact
Contact arrangements may have changed or there may be conflict regarding contact.
You may notice changes in parenting due to the impact of domestic abuse.
Adults and Family
There is a difference between an unhealthy relationship and domestic abuse. Domestic abuse is defined by one person having more power and control over another. There is likely to be disharmony and adults having arguments due to the stress of COVID-19
Isolation
If you have not seen a person you would normally see for a period of time, they may be isolated or they change how they contact you like using text or emails instead.
You may notice behaviour changes, less contactable, will ignore you on the street, no eye contact, wearing different clothes, long sleeves on a hot day
You may notice that the victim is always with the abusing adult and presents with different behaviours in their presence.
You may observe injuries
You may be aware that a victim or abusing adults’ mental health is deteriorating
Finance
Financial situation may change due to controlling and coercive behaviours, especially if the abusive partner has been furloughed or made redundant from work.
You may notice a victim using foodbanks or requesting additional benefits or financial assistance from agencies.
Alcohol and Drugs
You may see an increase in the use of alcohol or substances for the victim, abusing adult or young person
Children- Has this been a previous concern? If so, how has this been addressed?
- Talk to the child/young person to understand what it is like for them, using motivational interviewing to support this. This can be done through an activity together, talking, drawing or writing.
- Try and develop a safety plan with the child/young person, which includes where to get help in an emergency.
- Consider family and friends they have for support.
- Take a ‘Think Family’ approach.
Advice for working with parents and adults
- If there are children involved the person harming may use child contact to further control and abuse.
- If court orders are in place which are not being followed advise to contact the solicitor or police to enforce them.
- Be supportive of a person experiencing abuse who may be implementing their own safety plan while isolating with an abusing adult and for some may be managing parenting.
- For parents offer parenting advice but acknowledge that the parenting style is indicative of the situation.
- Offer early help support if there is an indication of impact upon the children/young person that is not safeguarding. (see more detail in LINK column).
- Advise to take regular breaks, walk around any outside space they might have, read a magazine, get the kids involved in an online exercise class.
- Show understanding regarding the stress caused by COVID-19 and offer advice and guidance regarding how to manage arguments.
Safety Planning
Basic principles:
- Keep a mobile phone charged and with credit.
- Call 999 in an emergency.
- Have a bag packed for emergencies that includes, important docs, money and clothes.
- Use the silent solution if needed.
- Encourage attendance at appointments to see professionals.
- Stay in touch with someone you trust, family/friends ask them to check in on you if safe.
- Use the you are not alone campaign safe nets at supermarkets ( details on open the door).
- Have a code word for safety.
- Can your employer offer you support?
- Use the Bright Sky and Hollie Guard apps. (see LINK column)
- Use safelives and women’s aid resources for safety planning information.
- Contact the Domestic Abuse Intervention and Prevention Service for support.
- Offer support regarding how to access additional funds.
- Support with opening own bank account if safe to do so.
- Utilise time at food banks if safe to contact domestic abuse services.
Is this ok?Children
- Support for children
- Support for young people
- CAFCASS preparedness
- CAFCASS guidance for children and families
- Family Lives
Adults
- Open the Door
- Safe Lives
- Surviving Economic Abuse
- Department for Work and Pensions: employment and benefits support
- National Debtline
- Citizens Advice
- Money Advice Service
Is this still ok?
Children
- Adults supporting children with domestic abuse
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- Silent solution
- Bright Sky App
- Hollie Guard App
- Freephone 24h National Domestic Abuse Helpline: 0808 2000 247
- LGBT+ Domestic Abuse Helpline: 0800 999 5428 help@galop.org.uk
- Galop Helplines
- Men’s Advice Line: 0808 810 327 info@mensadviceline.org.uk
- Respect – Men’s Advice Line
- Karma Nirvana, UK Helpline for ‘honour’-based abuse and forced marriage: 0800 5999 247
- Karman Nirvana Helpline
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Does the child/young person require urgent specialist support to address suicidal thoughts and behaviours?
- Children and Young Peoples Community Mental Health Services (previously CAMHS) consultation and referral when associated with changes in the behaviour e.g becoming more frequent or when accompanied with suicidal thoughts.
- Consider Accident and Emergency Department (999 or ensuring safe travel there) or Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
Safeguarding Concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Contact the Cheshire West Domestic Abuse Intervention and Prevention Service on 0300 123 7047 option 2.
- Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Drugs and alcohol
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Children
Young people may try drugs and/or alcohol for a number of different reasons:
- Peer pressure
- For fun
- Low mood
- Curiosity
- To help them to forget
- Self-medicate
- Boredom
- Lack of confidence
AdultsPeople use alcohol/ drugs for lots of reasons:
- To socialise
- To ‘escape’
- To fit in
- To experiment
Look out for:
- The person often feeling their need to have an alcoholic drink/ use drugs.
- Getting into trouble because of drinking/ drug use.
- Others warning them about how much they are drinking/ using drugs.
- The person themselves thinks their drinking/ drug use is causing problems.
ChildrenIs this something you were concerned about before?
Is the young person receiving professional support? Do they need to receive this?
Self-help: Via – Young People – Cheshire West and Chester
Signs to look for-
Is the Young Person-
- Mixing with new friends
- Experiencing moods swings
- Poor sleep patterns.
- Being secretive or evasive about where they’re going and what they’re doing
- Red-rimmed eyes and/or a runny nose
- Drowsiness
- Poor hygiene or appearance
- Loss of appetite
- Big increase in appetite
- An uncharacteristic loss of interest in school, hobbies and friends
- Money going missing regularly for no apparent reason
- Smelling of smoke or alcohol
- Returning home late and displaying unusual behaviour
- Slurred speech or rapid speech
- Dilated pupils
- Sudden dramatic weight Loss
- Health concerns/signs-
-Frequent sickness
-Nosebleeds
-Skin abrasions/bruises
-Sores around the mouth
-Headaches
How to respond- advice for parents/carers
- Talk to the young person open and honestly without judgement.
- Be a responsible role model.
- Set clear boundaries, structure and routines.
- Help your young person learn to make safe and healthy decisions.
- Support the young person to strengthen their sense of wellbeing in healthier ways – exercise, sport, music.
- Find out what you can about illegal drugs, their names, their effects, so that you can be well informed.
- Allow plenty of time, don’t rush the conversation.
- Respect what they have to say – don’t lose your temper,
- Let them know you’re there for them and that they can talk to you about drugs.
- If they are using, don’t confront them when they’re high.
- Seek professional support: Via – Young People – Cheshire West and Chester
Adults
Understanding why people use alcohol/ drugs helps us in our response:
- Some people use alcohol/ drugs occasionally to have fun, socialise and relax.
- Taking substances might not become a problem for these people, and they’ll probably stop when they’re ready to.
- You can appropriately make them aware that some drugs are illegal and can affect their physical and mental health.
- For some it is a way of escaping difficult feelings that they’re struggling to cope with.
- Some people take substances to fit in, or because they feel under pressure to do so by their friends. Talk to them and explore what interests and activities they enjoy that don’t involve alcohol/ drugs?
- Some people are just curious. They might try drugs once or twice to see what it’s like and then decide to leave it. Remember that most people who try drugs don’t continue using them.
- They might be feeling depressed, anxious, insecure and use alcohol/ substances/ to cope and manage their feelings. This will make these feelings worse for them.
- If you think this, talk to them, in an open and clam way, using trauma informed language and think about how motivational interviewing could support this conversation. Look out for ways to help them think about why they’re using alcohol/ drugs and ways they can manage without them. If necessary, suggest that they look for professional help.
Advice:
- Watch their alcohol consumption.
- The Government recommend for both men and women to have 2 alcohol free days a week and not to regularly drink more than 14 units a week. 14 units is equivalent to six pints of average strength lager ( 4% ABV) , or six medium size glasses of wine (175ml, 12% ABV).
- Seek support from a trusted person
- Find out more: Via – New Beginnings – Cheshire West and Chester
Is this ok?Children
Via – Young People – Cheshire West and Chester
Live Well Cheshire West and Chester – sign post drug and alcohol services
Adults
Via – New Beginnings – Cheshire West and Chester
Is this still ok?
Children
Find out how other services can help: Via – Young People – Cheshire West and Chester
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF).
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
– Multi agency group supervision
– Learning conversation - Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
Contact GP Practice they can offer advice and advise on the right treatment, this could be at the practice or a local service.
Contact Via – New Beginnings – Cheshire West and Chester the local service to help those affected by alcohol and substance misuse.(self-referrals or referrals by professionals can be made to this service)
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- New Beginnings is a fully integrated recovery service delivered by Via – New Beginnings – Cheshire West and Chester
- Email: cwac@wdp.org.uk
- Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
-
Displacement, War and Conflict
Recognise What you see … Respond What you can say and do … Link Where you can go for further advice,
support or do next …Displacement is a common after effect of war and conflict and is possibly one of the greatest humanitarian challenges of our time. When people become displaced, it is a traumatic experience, their physical, emotional and mental health often suffers.
The magnitude of displacement is broad and can encompass a number of different elements: the loss of a loved one, school routine and structure, unexpected endings, not taking exams, a job, not able to be with family and friends.
Many behaviours and experiences can be associated with displacement, war and conflict.
- Struggles eating and sleeping or comfort eating and sleeping a lot.
- Nightmares or night terrors
- Presentation of separation anxiety.
- Presentation of social anxiety – worried about going out and meeting others.
- Jumping in and out of feelings of loss, sadness and grief.
- Worried about death.
- Seeing changes in behaviour and emotions, could be seen as regressing in physical development for children or emotionally and socially for children and adults.
- Presenting angry, aggressive and controlling.
- Presenting as subdued and isolated.
- Reluctant to talk about feelings.
- Engaging in behaviours that cause harm.
- Not feeling safe and untrusting of others.
- Being dependant on support services for daily tasks.
- Struggle with decision making.
- Changes in routine leading to emotional dysregulation or challenging behaviours.
Children
Talking to children about the impact of loss:
- Lots of national and local support
- Have the child/young person and their family experienced loss and grief previously? Consider how this could be impacting further on them now.
- Prepare children before they return to school by using social stories.
– mainstream classroom
– comic strips - Children’s understanding of death at different ages
- Consider what supported them previously and if this would be appropriate to draw on again?
- Provide:
– re-assurance
– routine, structure and boundaries in place (knowing what to expect)
– warmth, comfort - “Normalising” feelings of loss, grief and anxiety
- Engaging children and young people in activities or with key people.
- Talking openly, naming the feelings and connections.
- Offering safe spaces to share, express, talk about feelings – personalise to child/young person’s needs (be creative: play, art, drama, dance, music, journaling, physical release, exercise, mindfulness, grounding).
- Talking factually about what’s occurred and impact (age appropriate).
- Allow short term dependence, regression.
- Encourage time with friends.
Adults
- Positive role-modelling.
- Engage in activities mentioned above.
- As and when helpful or needed support the adult in the above.
Is this ok?
Adults and children
- Migrant Help (migranthelpuk.org)
- Homepage – Refugees at Home
- Doctors of the World – Doctors of the World
- North West Regional Strategic Migration Partnership (northwestrsmp.org.uk)
- Home – Refugee Action (refugee-action.org.uk)
- Sunflower Sisters – Helping Ukrainian refugees settle in the UK (sunflowersistersforukraine.org)
- Home – Reset (resetuk.org)
- The British Red Cross | Worldwide Humanitarian Charity
- Home – Homes For Ukraine
- Information for families seeking refuge from war or conflict in their home country (beaconhouse.org.uk)
- Welcoming-Refugee-and-Asylum-Seeking-Learners.pdf (bell-foundation.org.uk)
- Mental health support for refugees and asylum seekers – Refugee Council
- Help for anyone fleeing the war in Ukraine | Helplines (barnardos.org.uk)
- Guidance for supporting the mental health and wellbeing of displaced Ukrainians – Thrive LDN
Children
- Can talk to school emotional literacy support assistant (ELSA) who can signpost/advise as required. It might be for six months to a year that children experience these emotions and behaviours.
- Mental health resource pack for schools.
- Understanding and Supporting Refugee Children and Young People by Dr Tina Rae, book resource being provided to all schools
- Managing unexpected endings and transitions
- Child Bereavement UK: supporting pupils
- Childhood Bereavement Network
- Grief Encounter
- Sesame Street – when families grieve
- Cruse Bereavement Care
- St Luke’s Children Bereavement Service
- Young Minds
- Child Bereavement UK
- Elsie Ever After
- Grief Encounter for bereavement support
- Hope Again
- UK Trauma Council – Traumatic Bereavement Resources
Adults
- Mind
- NHS Grief after bereavement or loss
- Adult Bereavement Service
- Mental health support for refugees and asylum seekers – Refugee Council
Is this still ok?
Children
- GP practice, public health nurse for advice and guidance.
- Reflect Children’s Bereavement Service
- Consider if further support can be provided through initiating a multi-agency Team Around the Family (TAF)
- If a TAF is in place does this need to be reviewed? Consider if a request for a learning conversation or multi agency group supervision would be appropriate:
- Multi-Agency Group Supervision
- Learning Conversations
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
Adults
- Advise to contact GP practice.
- Adult Bereavement Service
Am I still worried?
Children
Emotional health and wellbeing concerns:
- Consider Children and Young Peoples Community Mental Health Services (previously CAMHS) referral/consultation
- Counselling for emotional support
- Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485.
- Reflect Children’s Bereavement Service
Safeguarding concerns:
- Schools: if you have a safeguarding concern contact the Safeguarding Children in Education Team (SCIE)
- If you feel a child is at risk of harm speak to your designated safeguarding lead and contact i-ART on 0300 123 7047 (or out of hours 01244 977 277)
Adults
- Cruse Bereavement Care
- If concerns persist and/or increase contact Cheshire and Merseyside Mental Health Crisis Helpline on 0800 145 6485 and/or GP practice.
- Adult safeguarding concerns contact 0300 123 7034 (or out of hours 01244 977 277)
Development of this model has been led by the West Cheshire Children’s Trust, supported by the Safeguarding Children Partnership and Local Safeguarding Adults Board.